No products in the cart.
Uncategorized
Unlocking Your Mind: The Astonishing Neuroscience of Psychedelics
Introduction: Why Psychedelic Neuroscience Matters
The human brain is often described as the most complex structure in the known universe. For decades, psychedelics like psilocybin (magic mushrooms), LSD, and DMT were dismissed as recreational drugs or tied to counterculture movements. But today, cutting-edge neuroscience research is revealing how these compounds profoundly alter brain function, with implications for mental health, creativity, and spirituality.
In this article, we’ll dive into the neuroscience of psychedelics, explaining how they interact with the brain, why they hold therapeutic promise, and what science still has to uncover.
How Psychedelics Affect the Brain: A Scientific Overview
Advances in brain imaging have allowed scientists to observe real-time changes in brain connectivity and activity during psychedelic states. Here are the most significant findings:
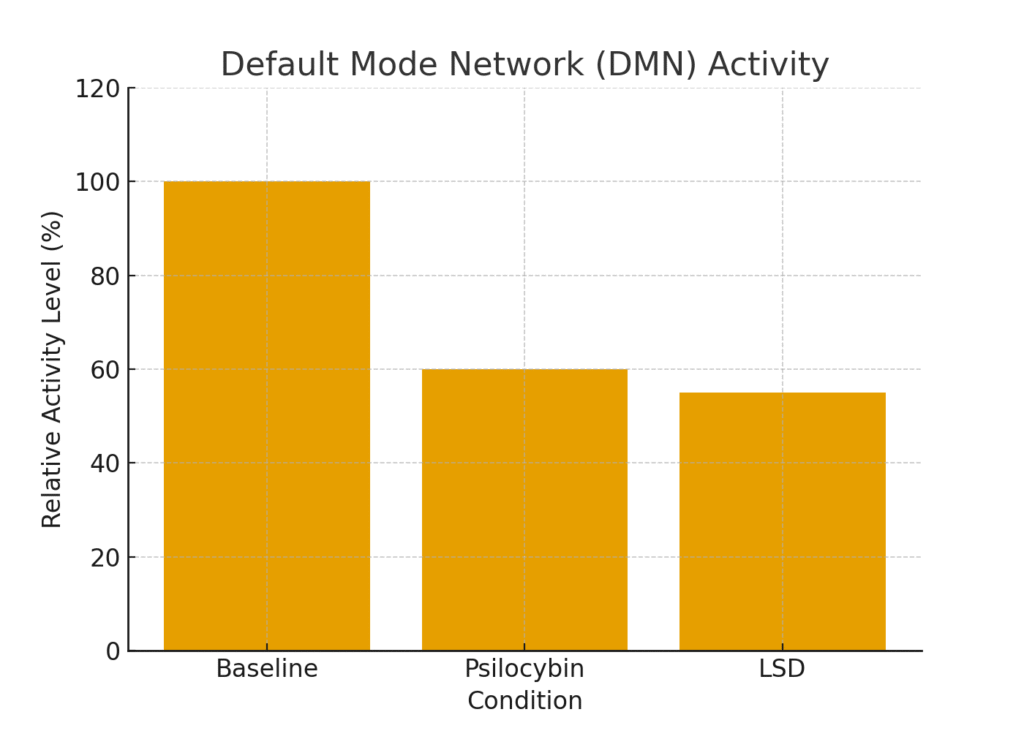
1. Default Mode Network (DMN) Suppression
The Default Mode Network (DMN) is a collection of brain regions responsible for self-reflection, autobiographical memory, and the sense of “self.” Overactivity in the DMN has been linked to depression and anxiety.
- Under psychedelics, DMN activity decreases, leading to “ego dissolution” and a reduced sense of rigid self-identity.
- This explains why patients often report feelings of oneness, interconnectedness, or spiritual awakening.
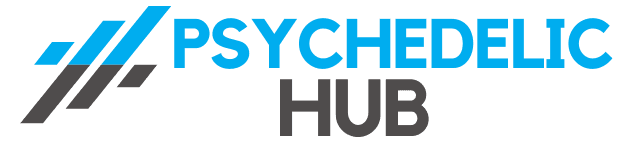
📊 Figure 1: Brain Connectivity Normal vs Psychedelic
2. Increased Global Brain Connectivity
Normally, the brain is organized into distinct networks (visual, auditory, motor, etc.), with limited cross-communication. Psychedelics temporarily break down these barriers.
- New neural pathways open up, allowing previously disconnected brain regions to “talk” to each other.
- This explains phenomena like synesthesia (hearing colors, seeing sounds) and enhanced creativity.
- Researchers describe this as a shift from a “rigid” brain state to a more entropic, flexible state.
3. Boost in Neuroplasticity
Psychedelics promote neuroplasticity — the brain’s ability to form new connections.
- Animal studies show psychedelics increase the growth of dendritic spines (tiny protrusions on neurons that facilitate communication).
- Human studies link psychedelic therapy to lasting improvements in mood, cognition, and behavior.
- This could explain why a single psychedelic session sometimes produces long-term relief from depression or PTSD.
📊 Figure 2: DMN Activity Before and After Psychedelics
Key Neurotransmitters Involved in Psychedelic States
Serotonin (5-HT2A Receptor)
Most classic psychedelics (psilocybin, LSD, DMT) primarily act on the 5-HT2A serotonin receptor.
- This receptor is critical for mood regulation, perception, and cognition.
- Overactivation leads to visual hallucinations, altered time perception, and expanded awareness.
Glutamate and Brain Plasticity
Psychedelics indirectly increase glutamate release, stimulating brain plasticity. This is particularly important in areas like the prefrontal cortex, which is linked to decision-making and emotional regulation.
Dopamine and Reward Systems
While not the primary target, psychedelics can enhance dopamine signaling, contributing to feelings of awe, novelty, and curiosity.
Psychedelics and Mental Health: The Healing Potential
The neuroscience of psychedelics isn’t just about trippy visuals — it’s about mental health breakthroughs. Clinical trials suggest psychedelics may revolutionize psychiatric treatment.
Depression
- Overactivity in the DMN is reduced, breaking cycles of negative rumination.
- A 2020 Johns Hopkins study found psilocybin-assisted therapy produced significant and sustained reduction in depression symptoms.
PTSD and Trauma
- Psychedelics enhance fear extinction and allow patients to revisit traumatic memories without overwhelming anxiety.
- MDMA-assisted therapy has shown groundbreaking results, with some patients no longer meeting PTSD criteria after treatment.
Addiction
- Psychedelics may “reset” reward pathways, disrupting addictive loops.
- Studies at NYU and Johns Hopkins show psilocybin therapy helps with smoking cessation and alcohol dependence.
Spiritual and Existential Insights
While the scientific community focuses on biology, many participants describe their experiences in spiritual terms:
- Mystical experiences often correlate with better therapeutic outcomes.
- Patients facing terminal illness report reduced end-of-life anxiety after psilocybin sessions.
- Neuroscience suggests that by quieting the DMN, psychedelics allow access to a non-ordinary state of consciousness often described as transcendent.
Ethical Considerations and Safety
Despite the promise, psychedelics are not a silver bullet. Important considerations include:
- Set and Setting: Psychological state and environment shape the experience.
- Dosage Control: Too much can lead to distress, confusion, or panic.
- Integration Therapy: Follow-up sessions help patients make sense of their experiences.
- Legal Status: Psychedelics remain illegal in many countries, though decriminalization is spreading.
Future Directions in Psychedelic Neuroscience
The field is moving quickly, with multiple FDA-approved clinical trials underway. Future research may answer questions like:
- Can psychedelics be tailored to target specific brain circuits?
- How do psychedelics compare to existing treatments like SSRIs or ketamine?
- Could psychedelics play a role in preventative mental health care?
The “psychedelic renaissance” is just beginning, and neuroscience will be at its core.
FAQs
Q1: How do psychedelics rewire the brain?
They promote neuroplasticity by growing new dendritic spines and enhancing cross-network communication.
Q2: Which part of the brain is most affected by psychedelics?
The Default Mode Network (DMN), associated with self-awareness and rumination, shows the most dramatic changes.
Q3: Are psychedelics safe for the brain long term?
Current evidence suggests no lasting brain damage in clinical settings, but misuse can cause psychological distress.
Q4: Can psychedelics replace antidepressants?
Not yet. Research is ongoing, and psychedelics are likely to be used alongside therapy, not as stand-alone drugs.
Conclusion
The neuroscience of psychedelics is unlocking new ways to understand the brain, treat mental illness, and explore consciousness itself. By suppressing the DMN, increasing brain connectivity, and promoting neuroplasticity, psychedelics hold the potential to transform psychiatry and wellness.
As science continues to explore these substances, the conversation is shifting from stigma to serious scientific inquiry — one that could change the future of mental health care.
References
- Johns Hopkins Center for Psychedelic & Consciousness Research
- MAPS (Multidisciplinary Association for Psychedelic Studies)
- Imperial College London Psychedelic Research Centre
- Carhart-Harris RL et al., Neural correlates of the psychedelic state, PNAS 2012